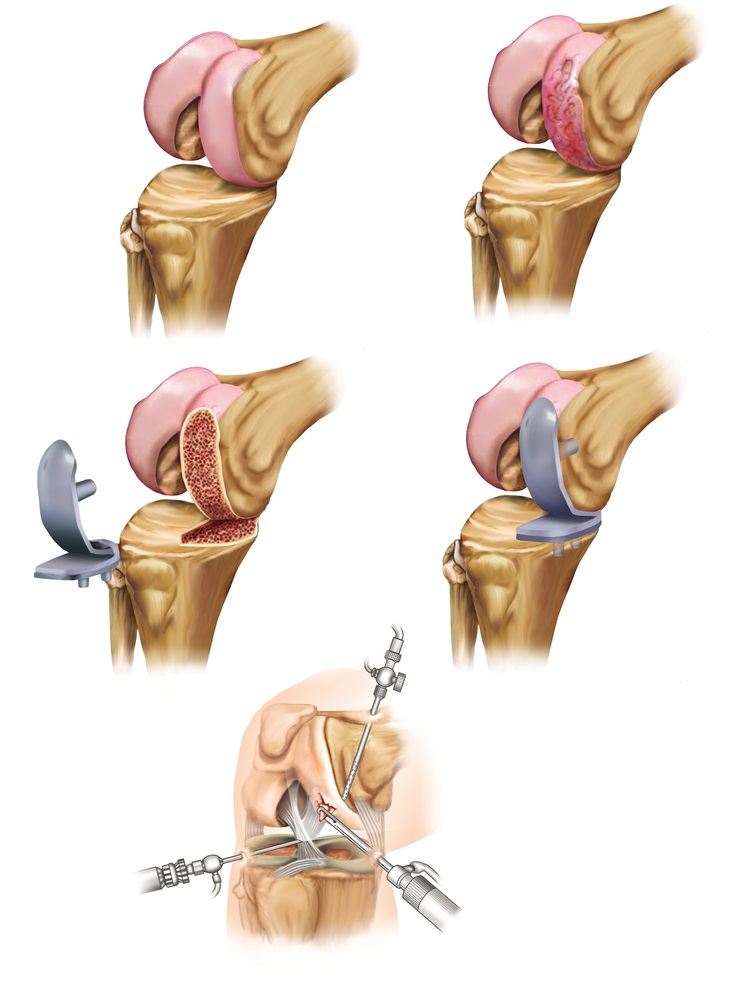
Partial Knee Replacement Surgery
Partial knee replacement, also known as unicompartmental knee arthroplasty (UKA), is a surgical procedure used to treat isolated areas of severe knee joint degeneration or damage. A native knee joint has three compartments: the medial compartment (inner side of the knee), the lateral compartment (outer side of the knee), and the patellofemoral compartment (behind the knee cap). If one of the three compartments is significantly worn out due to arthritis but the other two are very well preserved, partial knee replacement can be considered. Partial knee replacement involves replacing just one compartment out of the three. The components are made of alloys of cobalt and chromium for the femur and tibia, and a special plastic in the middle.
Advantages over total knee replacement surgery
– Quicker recovery in the initial post-operative phase: Surgery is less invasive and involves a smaller incision. Patients typically experience a faster recovery time after a partial knee replacement compared to a total knee replacement. Physical therapy and rehabilitation are often less intensive and may be required for a shorter period. The initial recovery period is approximately 3 to 4 weeks in most cases, as compared to 6 to 8 weeks for total knee replacement.
– Better range of motion: Most patients get 120 degrees of flexion or more after a partial knee replacement as compared to an average of 100-110 degrees of flexion after total knee replacement.
Disadvantages over total knee replacement surgery
Survivorship: The average survivorship of partial knee replacement is in the range of 8–10 years. Generally, after this period, either the rest of the knee joint develops progressive arthritis or components loosen or wear out, necessitating total knee replacement surgery
Ongoing pain/lack of full function: Some patients complain of ongoing pain or lack of full function after partial knee replacement due to some pre-existing arthritis in the other two native compartments of the knee joint.
Patient Selection
I choose my patients very carefully for partial knee replacement in order to achieve a successful outcome. This is done by careful history taking, focused clinical examination, and appropriate investigations. Investigations can include X-rays and occasionally MRI scans. In some cases, knee arthroscopy procedure may need to be carried out to assess the degree of arthritis in the joint and determine the suitability for partial knee replacement.
Physiologically young patients are best suited for this type of procedure; however, age is not the absolute criterion for partial knee replacement surgery.
Types of Partial Knee Replacement Surgery
The most commonly performed partial knee replacement involves replacing the medial compartment (inner part of the knee). Due to the biomechanics of the knee joint, the medial compartment of the knee develops progressive arthritis ahead of the other two compartments in the vast majority of the patients. Very occasionally, partial knee replacement of either the lateral compartment (outer part of the knee) or of the patellofemoral compartment (behind the knee cap) can be considered.
Based on how the bearing surface is fixed on to the components, partial knee replacement can be mobile-bearing or fixed bearing. However, studies have not shown any significant difference in clinical outcomes between the two types of knee replacement. In my practice, I use fixed bearing partial knee replacement.
Risks and Benefits
Overall, partial knee replacement is a very successful operation in modern-day surgery. In my practice, the success rate of a partial knee replacement is around 85-90%. Pain relief and improvement in the quality of life is substantial in the vast majority of patients. Partial knee replacement helps patients maintain an active life including sporting activities.
Risks of partial knee replacement include infection (around 1%), bleeding, DVT (clots in your leg), PE (clots in your lung), stiffness, loosening, wear, persistent pain (around 2-3%), need for further surgery, medical and anesthetic complications. Precautions are taken in order to minimize all the above risks e.g. use of antibiotic prophylaxis and specialized laminar airflow theatres to minimize the risk of infection, use of blood-thinning medications, and mechanical methods to reduce the risk of clots, etc. Post-operative exercises are extremely important to gain/maintain a good range of flexion after the surgery.
Rehabilitation and Recovery
You are generally admitted to the hospital on the day of surgery. The average length of stay in the hospital is 2-3 days. During the hospital stay, a multi-disciplinary team including an orthopaedic team, ward doctor, nursing staff, physiotherapist, and occupational therapist, treats you. Once you and the team are happy with the progress, you are discharged from the hospital.
Post-operative mobilization includes the use of walking aids like walkers or crutches, to begin with. You can subsequently use the walking stick/s until independent mobility can be achieved. Most patients can hope to regain independent mobility after 3-4 weeks.
You can expect some swelling and redness around the wound and of the lower leg for a few weeks. Generally, by 6 to 12 weeks, nearly full recovery can be expected in most patients. Most patients can expect to drive around 3-4 weeks mark.
Implants of My Choice
Currently, my preferred implants are PFC Sigma Higher-Performance Partial Knee System (manufactured by Depuy Synthes).
- Unicompartmental Knee Replacement
Copyright by FUW 2017-2024. All rights reserved.
