Total Knee Replacement Surgery
Knee replacement surgery is generally carried out for osteoarthritis of the knee. There are some other indications for this surgery including other types of arthritis, previous fracture, previous sporting injury, etc.
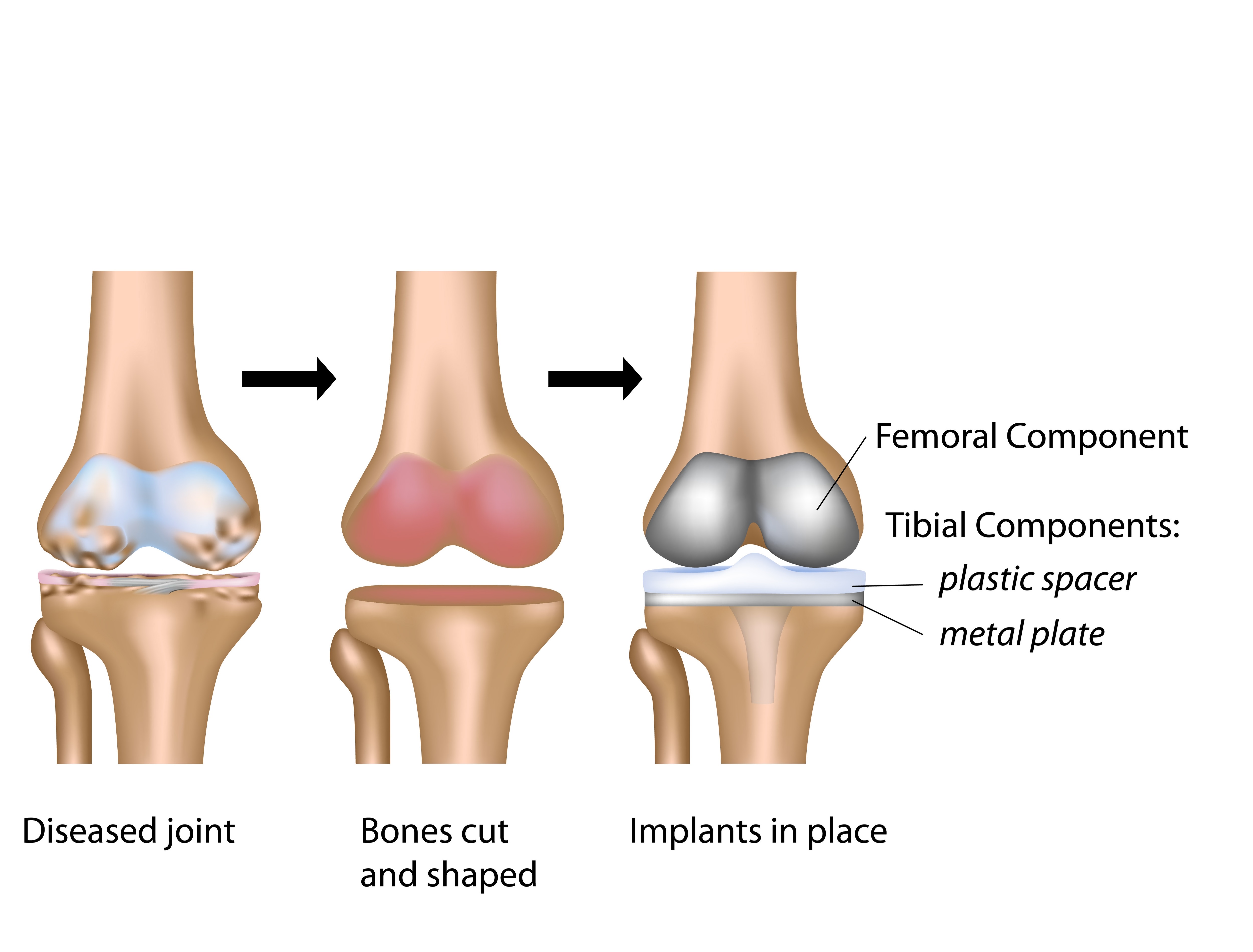
Knee replacement surgery involves removing the damaged joint surfaces from both sides of the joint (from femur and tibia) and preparing the joint surfaces in order to accommodate an artificial joint. The artificial joint is matched to the patient’s size using specialized instruments and trial components.
Types of Knee Replacement
Knee replacement generally consists of a metal femoral component (made out of cobalt and chromium alloy), metal tibial component (made out of either titanium or cobalt and chromium alloy) and a plastic (highly cross-linked polyethylene) in the middle. The bearing surface therefore is metal on plastic.
Based on how the bearing surface is fixed on to the components, knee replacement can be mobile bearing or fixed bearing. However, studies have not shown any significant difference in clinical outcome between the two types of knee replacement. In my practice, I use fixed bearing total knee replacement.
Based on the number of ligaments preserved during the surgery, knee replacement can be classified into cruciate-retaining (preserving posterior cruciate ligament) and cruciate sacrificing (removing posterior cruciate ligament). Although this largely depends on the surgeon’s preference, studies have not shown any significant difference between these two types of knee replacement. In my practice, I generally use cruciate-retaining knee replacement for most cases.
Risks and Benefits
Overall, total knee replacement is a very successful operation in modern-day surgery. In my practice, the success rate of a total knee replacement is 90% or higher. Pain relief and improvement in the quality of life is substantial in the vast majority of patients. It improves mobility and alleviates pain during day-to-day activities. It also helps patients maintain an independent life with little/no dependence on carers/family.
Risks of total knee replacement include infection (around 1%), bleeding, DVT (clots in your leg), PE (clots in your lung), stiffness, loosening, wear, persistent pain (around 1%), medical and anesthetic complications. Precautions are taken in order to minimize all the above risks e.g. use of antibiotic prophylaxis and specialized laminar airflow theatres to minimize the risk of infection, use of blood-thinning medications, and mechanical methods to reduce the risk of clots, etc. Post-operative exercises are extremely important to decrease the risk of post-operative stiffness.
Rehabilitation and Recovery
You are generally admitted to the hospital on the day of surgery. The average length of stay in the hospital is 3-4 days. During the hospital stay, a multi-disciplinary team including an orthopedic team, ward doctor, nursing staff, physiotherapist, and occupational therapist, treats you. Once you and the team are happy with the progress, you are discharged from the hospital.
Post-operative mobilization includes the use of walking aids like walkers or crutches, to begin with. You can subsequently use a walking stick/s until independent mobility can be achieved.
You can expect some swelling and redness around the wound and of the lower leg for a few weeks. Generally, by 6 to 12 weeks, functional recovery can be expected in most patients. Most patients can expect to drive around 6 weeks mark.
Implants of My Choice
I choose the implants for knee replacement very carefully for each patient. The type of knee replacement used in my clinical practice has a very long track record (>20 years) with excellent long-term survival. Currently, my preferred implants are PFC Sigma (manufactured by Depuy Synthes) and Nexgen (manufactured by Zimmer).
- Artificial Joint Replacement of the Knee
- Osteoarthritis of the Knee
- Viscosupplementation for Osteoarthritis of the Knee
Copyright by FUW 2017-2024. All rights reserved.
